The ACCESS Health Digital (AHD) Stamp of Confidence (SoC) for Digital Health Systems is a voluntary program. It is established by AHD to provide for a Stamp of Confidence for Digital Health Systems. Criteria for SoC are established as per as per NDHB Standards and related building blocks notified by Govt of India. The SoC Program supports the availability of quality Digital Health systems for its encouraged and required use across the National Digital Health Ecosystem. The SoC Program is run as a third-party product conformity assessment scheme for Digital Health systems based on the principles of the NDHB, EHR and MDDS for Health and Meity Open Standards and Opensource policy.
Download: Stamp of Confidence Stages and Criteria
As a part of its Social Entrepreneurship Accelerator (SEA) program designed to guide the healthcare industry in adopting open and uniform digital health standards, ACCESS Health Digital recently launched the Stamp of Confidence initiative that will recognize health startups based on the extent of their adoption of globally applicable digital health standards.
The Stamp of Confidence (SoC) is an endorsement issued to each of the SEA members based on the extent and depth of their compliance, placing them in different stages of compliance maturity. It is a mark of accomplishing technical and functional compliance to the recommended standards laid out in the National Digital Health Blueprint.
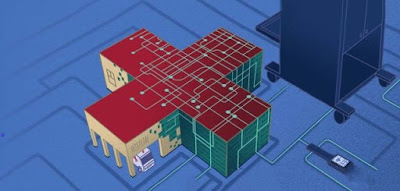
The SoC is structured in a way that helps startups transition gradually and smoothly from nonstandard healthcare industry to a standardized, open yet secure industry. The idea is to accelerate the adoption of the National Digital Health Blueprint standards and other Government of India notified digital health standards (including Metadata and Data Standards, SNOMED, Electronic Health Records, and Fast Healthcare Interoperability Resources) in a systematic and progressive way to make National Digital Health Ecosystem a reality.
The SoC has been adopted by the National Health Authority’s- Market Access Program (MAP) to bring in a structured approach to compliance and adoption under the Pradhan Mantri Jan Aarogya Yojana (PMJAY). ACCESS Health Digital is among the leading partners of the NHA under the MAP.
The SEA program run by ACCESS Health Digital is aimed to help Indian HealthTech startups and vendors implement Open Digital Health Standards that are applicable globally. With the introduction of the Minimum Viable Product [MVP], ACCESS Health Digital seeks to address the absence of interoperability between members of this vast ecosystem, which has been impeding the scale and speed of data and knowledge flow that are vital to achieve universal health coverage. The dedicated effort in this direction includes:
Minimal Viable Product Definitions (MVP): For various care delivery settings across primary, secondary, tertiary and health insurance segments.
Techno-functional evaluation and mentorship: To provide technical and functional mentorship for the implementation of the Minimal Viable Products (MVPs) into the partner products and to help build the micro services and Application Programming Interface (APIs) together with the product teams of the SEA community.
AHD Stamp of Confidence: At the end of the mentorship, the startups are assessed objectively against the custom recommendations provided for them during their initial techno-functional evaluation. The SoC milestone is recognized with the issuance of the Stamp of Confidence which certifies the area and stage of compliance.
Tiered Compliance Stages
The tiered approach of the Stamp of Confidence enables startups to join the network even when they are successful in implementing only the early “terminology standards”; thus giving them an opportunity to participate in the digital ecosystem. Early adopters in the stage 1 category are expected to implement other standards such as audit trails, Health Data Dictionary and pay attention to scalability along with the implementation of terminology standards. Also, every stage in the tiered system has room to accommodate anomalies or exceptions as the healthcare technology market is characterized with high degree of diversity in digital maturity, thus highlighting ‘inclusiveness’ in its design.
Stage 2 expects the startups to come forward to implement the eObjects and microservices which requires significant amount of commitment to interoperability and scalability in design. Stage 3 is conferred on those advanced players who can demonstrate the implementation of Data privacy and security principles in their design owing to the fact that they have the required data standards and terminologies implemented to enable them to achieve this stage.
Once the startups have completed their mentorship phase and are ready to be considered for the SoC, they are evaluated objectively using a techno-functional checklist which allows them to be scored against a stepwise implementation of every component within the specific stage.
Achieving a score ‘4/5’ in this objective assessment qualifies the startup to be considered ‘compliant’. Implementation of these standards in real world is the demonstration of excellence and provides them with a score ‘5/5’.
The Social Entrepreneurship Accelerator Program (SEA) strongly positions the early adopters of standards in its network as National Digital Health Blueprint (NDHB) Standards compliant products and the SoC is a major milestone that is required for the members to graduate to the coveted Early adopters club. Some of the early adopters in the SEA community like Plus91, Srishti Soft, UNIMEDNET, MarSha, Raxa, Invoker Tech, DocEngage have been identified and recognized to be the champions, leading the way in this journey. Saathealth, an MAP member has been one of the first few to receive the Stamp of Confidence. With greater and faster adoption of standards, other MAP members are expected to follow suit.
http://www.openbodhik.in/2020/07/social-entrepreneurship-accelerator.html